Periodontal disease is more commonly known as gum disease and was referred to as pyorrhea in the old days. It is a progressive inflammatory disease of the gingival and the surrounding tissue (bone) around the teeth.
Periodontal disease is the number one cause of tooth loss after the age of 30 and it is believed that around 80% of the population above the age of 30 may suffer from this disease, with varying degrees of severity.
It is usually painless and is mainly caused by plaque although pregnancy, diabetes, epilepsy, and such medications as chemotherapy, medication prescribed for heart problems, birth control pills, and antidepressants can all make you more susceptible to gingivitis which is one of the more common forms of periodontal disease.
Treatment will depend upon the type of periodontal disease and how far the condition has progressed.
There are many forms and stages of periodontal disease.
The most common are:
Gingivitis
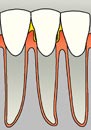
The first stage of periodontal disease, gingivitis, is the mild inflammation of the gingival caused by plaque build up. Your gingival will be red, swollen, and tender. You may also notice bleeding while you brush and floss. This stage of periodontitis is reversible.
Mild Periodontitis
Inflammation will spread to the supporting alveolar bone. Minor bone loss and the formation of periodontal pockets, or food traps, may occur.
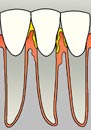
Moderate Periodontitis
In this stage, there will be increased gingival recession, moderate to deep pockets, moderate to severe bone loss, and mobility of teeth due to the bone loss.
Severe Periodontitis
This is the most serious stage of periodontitis. Deep pockets, increased mobility of teeth, movement of teeth out of position, and visible fistulas (boils) will be present in this stage. Pus may develop; bone loss continues, and your teeth may loosen or fall out.


Missing Tooth and Receding Gum Tissue
Diagnosis

To diagnose periodontal disease, several findings should be evaluated:
- Color and condition of the gum line
- Pocket depth measurements
- Bone line as revealed by x-rays
- Mobility of teeth
- Amount of calculus
These findings determine the periodontal disease stage and therefore determine the appropriate treatment plans
Treatments
- Non Surgical Treatment
- Surgical Treatment
Non Surgical Treatment
- Gingivitis
- Mild Periodontitis
Prevention
The best way to prevent periodontal disease and tooth decay is to maintain good oral health care. Brushing your teeth every day will remove a thin sticky film of bacteria, called plaque that grows on your teeth. Cleaning between the teeth once a day with floss removes plaque from between the teeth – areas where the toothbrush can’t reach. Brushing and flossing are essential in preventing gum disease. Brush your teeth twice a day, with a soft-bristled brush. Use a formula of toothpaste that contains fluoride, which helps protect your teeth from decay. It is also advisable to seek regular dental visits that include a periodontal evaluation.
Non Surgical Treatments
Oral Hygiene
If the disease is still in the first stage (gingivitis) your dentist may prescribe an anti-microbial mouth and advise you to brush and floss on a regular basis.
Dental Prophylaxis
Treatment for the prevention of periodontal diseases or other dental diseases by the cleaning of the teeth in the dental office using the procedures of Dental Scaling and Polishing. The treatment may include plaque detection, removal of supra- and subgingival plaque and calculus, application of caries-preventing agents, checking of restorations and prostheses and correcting overhanging margins and proximal contours of restorations, and checking for signs of food impaction.
Scaling
Scaling is procedure that meticulously removes contamination toxins, micro-organisms, plaque, tartar, cementum, dentin that is rough and/or permeated by calculus from around, below and under the gum line down to the bottom of the pocket. This is done to remove biofilm, calculus, and toxin down to the bottom of each periodontal pocket in order to obtain a healing response.
Root Planing
Root planing involves smoothing the root surfaces of your teeth with thin curettes so gum tissue can more firmly reattach to roots that are clean and smooth to prevent tooth loss and sensitivity problems. The procedure makes it more difficult for plaque to accumulate along the root surfaces. Because this procedure goes deeper than a regular cleaning, your mouth may be numbed. The cleaning may take two visits to complete. Depending on the extent of the disease you may need one or more sections (quadrants) of the mouth to be treated with scaling and root planing. Treatment may require one or more visits.
Scaling and Root Planing
Periodontal scaling is a treatment procedure which involves the instrumentation of the crown and root surfaces of the teeth. Plaque, calculus, and stains will be removed from these surfaces. It is performed on patients with periodontal disease and is therapeutic, as apposed to prophylactic and may precede root planning. It is a definitive, meticulous treatment procedure aimed at the removal of cementum and/or dentin that is rough and is possibly permeated by calculus, or even contaminated with toxins or microorganisms. When carried out thoroughly, some unavoidable soft tissue removal occurs. This procedure can be used as a definitive treatment or as part of pre-surgical therapy (“tissue preparation”) depending on how far the periodontal disease has advanced. Debriding the root surface is a critical element in establishing periodontal health.
Surgical treatments (moderate & severe periodontitis)
Gingivectomy
You may need surgery for severe gum disease (periodontitis) if it cannot be cured with antibiotics or root planing and scaling. A gingivectomy removes and reshapes loose, diseased gum tissue to get rid of pockets between the teeth and gums. A gum specialist (periodontist) or oral surgeon often will do the procedure. The Periodontis will start by numbing your gums with a local anesthetic. The Periodontis may use a laser to remove loose gum tissue. After removing the gum tissue, the doctor will put a temporary putty-like substance over your gum line. This will protect your gums while they heal. You can eat soft foods and drink cool or slightly warm liquids while the putty is in place and your gums are healing.
Periodontal Flap Surgery
Periodontal Flap Surgery, which is also called pocket depth reduction, your periodontist folds the gum back away from the tooth. Periodontal Flap surgery is recommended in many cases where pocketing depths have reached a level that makes maintenance or cleansing difficult. It is often associated with areas of bone loss and inflammation of the gum tissue around the teeth.
When scaling and root planing have been unsuccessful in eliminating the entire pocket of decay, or when there has been bone loss that needs to be surgically corrected, then a dentist may perform periodontal flap surgery. In flap surgery, under local anesthesia, small incisions are made in the gum, so that it can be lifted back to expose the tooth and bone. The entire area is carefully cleaned and all tarter and infected granulation tissue are removed and the bone is examined. Because periodontal disease causes bone loss, often the bone will need to be re-contoured in order for the gum to heal properly.
After scraping away the bacteria-laden plaque and tartar, the dentist removes diseased tissue and smoothes the surface of damaged bones. Then the dentist sews the tissue back into place. Removing or smoothing damaged tissue allows the gum tissue to better reattach to healthy bone.
Soft & Hard Tissue Grafts
Soft tissue grafts can be used to cover roots or develop gum tissue where absent due to excessive gingival recession. A thin piece of tissue is grafted from the roof of the mouth, or gently moved over from adjacent areas, to provide a stable band of attached gingiva around the tooth. The gingival graft may be placed in such a way as to cover the exposed portion of the root. During this procedure, the periodontist takes gum tissue from your palate or another donor source to cover the exposed root. This can be done for one tooth or several teeth to even your gum line and reduce sensitivity.
Hard tissue grafts in cases of gum recession a graft is usually taken from the palate and transplanted onto the affected area. This reinforces the thin gum and makes it difficult for the gum to recede further and may even help to cover the exposed root. It may also reduce tooth sensitivity and even improve the esthetics of your smile.
Scaling and Root Planing
Periodontal scaling is a treatment procedure which involves the instrumentation of the crown and root surfaces of the teeth. Plaque, calculus, and stains will be removed from these surfaces. It is performed on patients with periodontal disease and is therapeutic, as apposed to prophylactic and may precede root planning. It is a definitive, meticulous treatment procedure aimed at the removal of cementum and/or dentin that is rough and is possibly permeated by calculus, or even contaminated with toxins or microorganisms. When carried out thoroughly, some unavoidable soft tissue removal occurs. This procedure can be used as a definitive treatment or as part of pre-surgical therapy (“tissue preparation”) depending on how far the periodontal disease has advanced. Debriding the root surface is a critical element in establishing periodontal health.




